Massachusetts is arguably the most procedurally complex state for debt collection in New England. Unlike other states where a court judgment automatically grants you the right to garnish wages, Massachusetts requires a second, tedious legal battle known as “Supplementary Process.”
If your current agency thinks getting a judgment means “mission accomplished,” they are likely sitting on a pile of uncollected paper judgments. In the Commonwealth, a judgment is just a piece of paper until a judge issues a specific “Payment Order”.
For revenue cycle leaders—from the academic medical centers in Boston to community hospitals in the Berkshires—this means you need a partner who doesn’t just know how to sue, but how to navigate the post-judgment maze of M.G.L. c. 224.
Need a Medical Collection Agency in Massachusetts? Contact us
Deep Analysis: The 3 Revenue Traps in the Commonwealth
Standard national strategies fail here because they underestimate the protections built into the Massachusetts General Laws (MGL) and Attorney General regulations (940 CMR 7.00).
1. The “Supplementary Process” Bottleneck
-
The Law: Winning a lawsuit (M.G.L. c. 218) does not give you the right to garnish wages immediately. You must file a separate “Supplementary Process” action (M.G.L. c. 224) to bring the debtor back to court for an “examination of ability to pay.”
-
The Risk: Most agencies stop after the first lawsuit. They get the judgment and wait for a check that never comes. Without the “Supplementary Process” order, the debtor has zero legal obligation to hand over their paycheck.
-
Our Solution: We treat the initial judgment as merely “Step 1.” Our legal workflow automatically triggers the Supplementary Process filing if a voluntary plan isn’t reached within 30 days of judgment, forcing the debtor to disclose their assets to a judge.
2. The “Health Safety Net” (HSN) Compliance Trap
-
The Law: Massachusetts hospitals are required to screen patients for the Health Safety Net (HSN) (formerly the Free Care Pool) before billing. Eligibility extends up to 300% of the Federal Poverty Level.
-
The Risk: If you send an account to collections without properly documenting this screening, you aren’t just violating MassHealth regulations—you risk losing your surcharge reimbursements from the state pool.
-
Our Solution: We integrate an “HSN Scrub” into our intake. If a patient flags as potentially eligible (e.g., unemployed or on MassHealth Limited), we pause collection and help you route them back to your financial counselors, often recovering payment from the state rather than the patient.
3. The “70A Lien” Timing Rule
-
The Law: M.G.L. c. 111 § 70A allows you to place a lien on a patient’s personal injury settlement. However, the lien must be perfected prior to any judgment or settlement.
-
The Risk: Unlike states with a “100-day post-discharge” window, Massachusetts requires strict timing. If the patient settles their accident case on Tuesday and your agency files the lien on Wednesday, your lien is worthless.
-
Our Solution: We monitor “Date of Accident” vs. “Current Date” closely. We file Notice of Liens via certified mail immediately upon identifying third-party liability to “lock in” your claim before the insurance company cuts a check.
Nexa provides 100% reputation-safe, equipped with all 50-state collections license, offering free credit reporting, free litigation, free bankruptcy scrubs, and zero onboarding fees. Secure – SOC 2 Type II & HIPAA compliant. Over 2,000 online reviews rate us 4.85 out of 5.
Need a Collection Agency? Contact us
Our 4-Step “Bay State” Recovery System
We have adapted our model to handle the 940 CMR 7.00 regulations and the specific “capias” (arrest warrant for civil contempt) procedures unique to MA.
Phase 1: HSN & Insurance Audit (Pre-Collection)
-
The Strategy: We verify if the patient is an HSN candidate. We also check for Auto Insurance (PIP) on accident claims, as MA is a “No-Fault” state where the auto insurer pays the first $2,000 or $8,000 of medical bills before health insurance touches it.
Phase 2: The “940 CMR” Compliant Nudge (Steps 1 & 2)
-
The Strategy: Massachusetts has strict rules on call frequency (no more than 2 calls in 7 days to a home). We use a “Letter-First” approach that respects these limits while clearly explaining the debt.
-
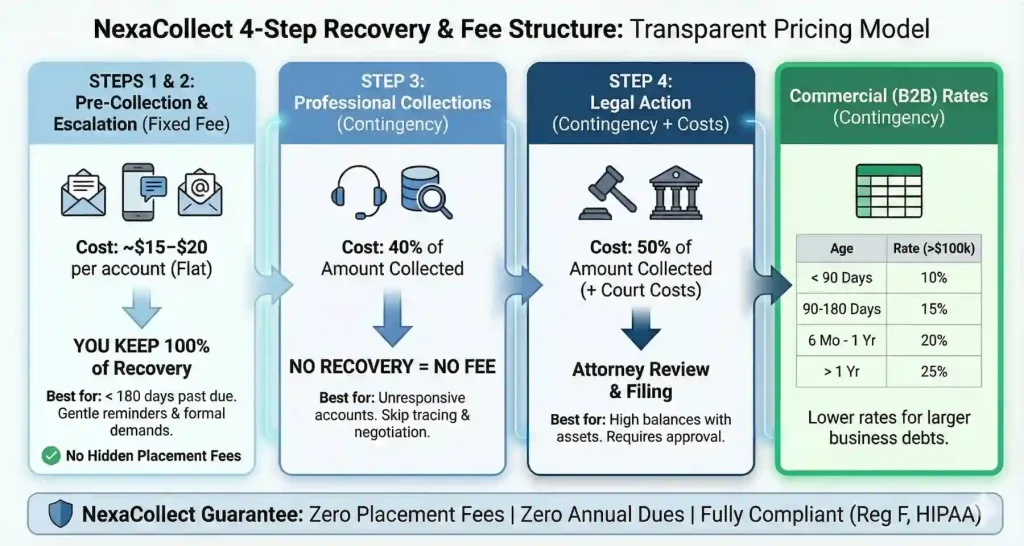
The Cost: Flat fee (approx. $15/account). You keep 100% of recoveries.
Phase 3: The “Payment Order” Negotiation (Step 3)
-
The Strategy: We explain the reality of M.G.L. c. 224 to the debtor. “Mr. Smith, if we go to Supplementary Process, the judge will examine your spending—coffee, cable, rent—and order a weekly payment. Let’s set up a voluntary plan now to keep you out of court.”
-
The Cost: 40% contingency.
Phase 4: Litigation & Capias (Step 4)
-
The Strategy: We use the courts not just for a judgment, but for enforcement. If a debtor ignores the Supplementary Process order, we petition for a Capias (civil arrest warrant) to compel their appearance. This is the “nuclear option” that usually prompts immediate payment.
-
The Cost: 50% contingency.
Regional Strategy: Serving the Commonwealth
Collecting in Boston is different from collecting in Worcester. We adjust our tactics accordingly.
| Region | Economic Profile | Collection Strategy |
| Greater Boston (MGB/Beth Israel) | High Income / Biotech | Focus on insurance denials and “balance billing” disputes. Patients here are savvy; we use detailed EOB explanations to prove the debt is valid. |
| Central MA (UMass Memorial) | Mixed Industrial / Ed | High volume of “underinsured” patients. We use flexible payment plans that align with bi-weekly factory or university payroll cycles. |
| Western MA (Baystate) | Rural / Service | HSN eligibility is higher here. We focus heavily on screening for state assistance to ensure we aren’t chasing uncollectible debts. |
FAQ: The Executive Summary
Q: Can you garnish wages in Massachusetts?
A: Yes, but it is harder than in other states. We can garnish the lesser of 15% of gross wages or the amount exceeding 50x minimum wage. However, we must get a Supplementary Process order first. It is a two-step legal battle.
Q: What is the Statute of Limitations?
A: You have 6 years to sue for medical debt (contract actions). However, we recommend acting within 12 months to ensure we can leverage insurance appeals if needed.
Q: Can you charge interest?
A: Generally, yes. The statutory rate is 6% unless your admission paperwork specifies a different rate. If you try to charge more without a contract, you risk violating state consumer protection laws (c. 93A).
Click here for a Free Audit of Your Massachusetts Bad Debt