Healthcare, like almost every other business area, deals with a lot of user-sensitive data.
Unlike many other commercial activities, providing medical services means knowing how to handle and store this highly sensitive information. Physicians and other care providers have several considerations when managing their patient data, ranging from legal compliance to cybersecurity. And data management isn’t only about ensuring that the information is secure; it ultimately can provide opportunities for greater care through insights and data analysis. Let’s take a quick look at some helpful ways healthcare providers can protect, manage, and leverage patient data.
HIPAA Legal compliance
HIPAA (Health Insurance Portability and Accountability Act) was enacted in the U.S. in 1996 to protect patient health information. It includes rules and regulations that healthcare providers, including doctors, must follow to be compliant. Here are some of the key components of HIPAA compliance:
-
Privacy Rule: The Privacy Rule restricts who can have access to Protected Health Information (PHI). PHI includes a broad array of information, from the individual’s past, present, or future physical or mental health conditions, to the provision of health care and payment for that care. Doctors must have safeguards in place to protect this information and can only disclose it under specific conditions.
-
Security Rule: The Security Rule stipulates that doctors must have physical, technical, and administrative safeguards in place to protect electronic PHI (e-PHI). This can include secure computer systems, locked file cabinets for paper records, and policies to handle data breaches.
-
Breach Notification Rule: If there is a breach of unsecured PHI, the doctor must notify the individuals affected, the Department of Health and Human Services (HHS), and in some cases, the media.
-
Enforcement Rule: This rule provides guidelines for investigations into compliance. If a doctor is found to be in violation of HIPAA, they could be subject to penalties.
-
HITECH Act: The Health Information Technology for Economic and Clinical Health (HITECH) Act was enacted as part of the American Recovery and Reinvestment Act of 2009, and expands upon the original HIPAA legislation. Among other things, it increases penalties for HIPAA violations and extends some of the requirements of HIPAA to business associates.
HIPAA violations can be quite costly for providers, with maximum penalties for noncompliance of 1.5 million dollars per incident.
The role of data in healthcare
The digitization of medical records is far from new, with electronic health records (EHRs) being the norm in the industry for many years. Physicians and other providers collect, store, and share digital patient records, and the number of records continues to grow. The widespread use of EHRs has resulted in large data sets.
To ensure HIPAA compliance, doctors should do the following:
- Risk Analysis and Management: Regularly perform risk analysis to identify potential vulnerabilities to the confidentiality, integrity, and availability of e-PHI.
- Training: Regularly train all staff members about the importance of HIPAA compliance and how to follow the rules.
- Policies and Procedures: Develop and implement clear policies and procedures to comply with the Privacy, Security, and Breach Notification Rules.
- Business Associates Agreement (BAA): Ensure that any third parties that may handle PHI on your behalf (known as “business associates”) are also compliant with HIPAA regulations. This is often handled through a BAA.
- Access Control: Limit access to PHI to only those employees who need it to perform their job duties.
- Data Encryption: Encrypt e-PHI, both at rest and in transit, to protect it from unauthorized access.
One reason for this growth is the use of connected devices for delivering care and monitoring patient well-being. Internet of Things (IoT) devices connect patients with care providers and collect data that can help diagnose and monitor patient health.
This increased data has been shown to reduce hospital-acquired conditions and increase cost savings through innovations in billing, bundled payments and debt collection. Data can undoubtedly improve the quality of care, but it can also overwhelm providers. Data burnout is a growing problem with providers because all of the information leads to overwork. Cumbersome health records software is a culprit, and so, is the often puzzling and complicated process of navigating insurance reimbursements.
Cybersecurity practices for providers
Data security is one of the most significant risk areas of concern under HIPAA. All businesses need to pay close attention to cybersecurity. But the vast amount of collected data in healthcare, the sensitive nature of that data, and the consequences of noncompliance means that healthcare providers have to be especially vigilant. Also, cybercriminals are only getting more sophisticated, with new, unknown threats developing on a near-daily basis.
Today, delivering healthcare means providing security for patient data. Cybersecurity is not just a technical concern, it is a patient safety issue. Providers rely on health IT vendors, adding a layer of complexity, and it has become clear that while HIPAA provides a basic framework for data protection, it is not sufficient in today’s data-heavy world.
This last practice may be the most effective, as human error is most often the culprit in data loss. For example, if a person uses the same username and password combination across multiple digital services, the risk of compromised credentials skyrockets. This is because cybercriminals have had so much success in data breaches that collect user login information. So, suppose a banking login is stolen, and the same combination of credentials is used for logging into an EHR system. In that case, it’s entirely possible that a hacker would attempt logging in with the credentials. This is because vast amounts of compromised login data exist.
To avoid this one major problem, organizations can educate users on password policies and how to recognize such threats as phishing emails.
Overall, data management can be an obstacle to the delivery of care and can affect the business of healthcare. Providers should prioritize data management, as it can lessen the burden of modern medical practice, ensure compliance, and protect patient data.
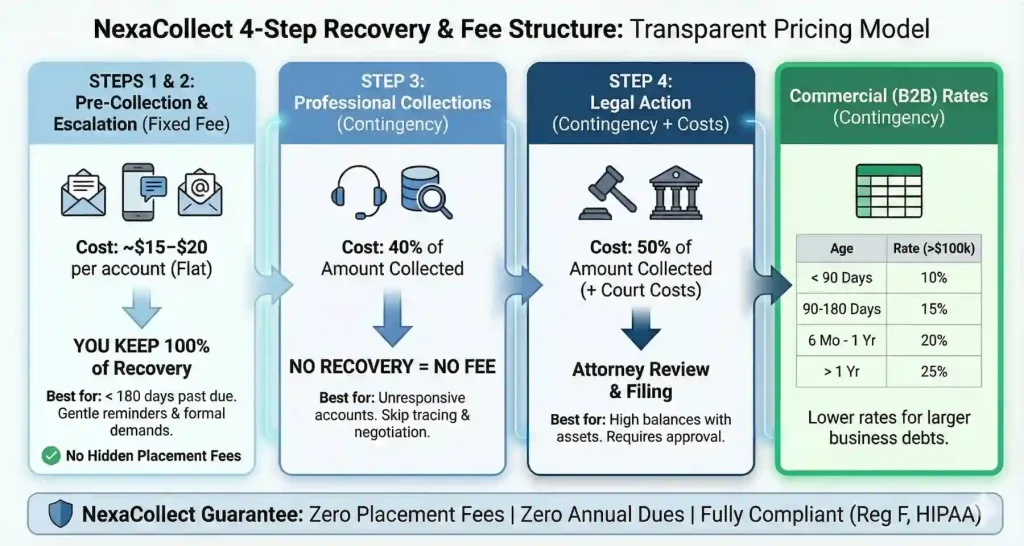
Nexa has assisted several hospitals and medical professionals to recover money from their past due accounts effectively. If you need a debt collection agency: Contact us