Healthcare clinics that wish to succeed in today’s competitive market must strive not only to provide quality care while keeping up with the continual technological advances of such a fast-paced and innovative industry but also to ensure they are managing their costs effectively.
The healthcare market is growing bigger every year – according to the Bureau of Labor Statistics, the number of healthcare clinics opening each year is steadily rising, with healthcare jobs predicted to increase 30 to 40 percent over the next ten years.
When a business implements a cost-optimization plan, there are a few key areas that need careful consideration: cost and pricing evaluation, process and service optimization, and streamlining of system operations. A healthcare clinic is no different, and the principles of lean methodology can be applied to any clinic’s cost optimization plan – adjusting the staff, resources, effort, and energy to guarantee best value for patients.
Optimizing the skills of your staff
Like any business, healthcare clinics will have a wide range of expenses that owners need to cover. From administrative costs to payroll and marketing, the expense categories can vary widely depending on the type of clinic. Here is a general overview of the main areas that can be analyzed in terms of cost-optimization.
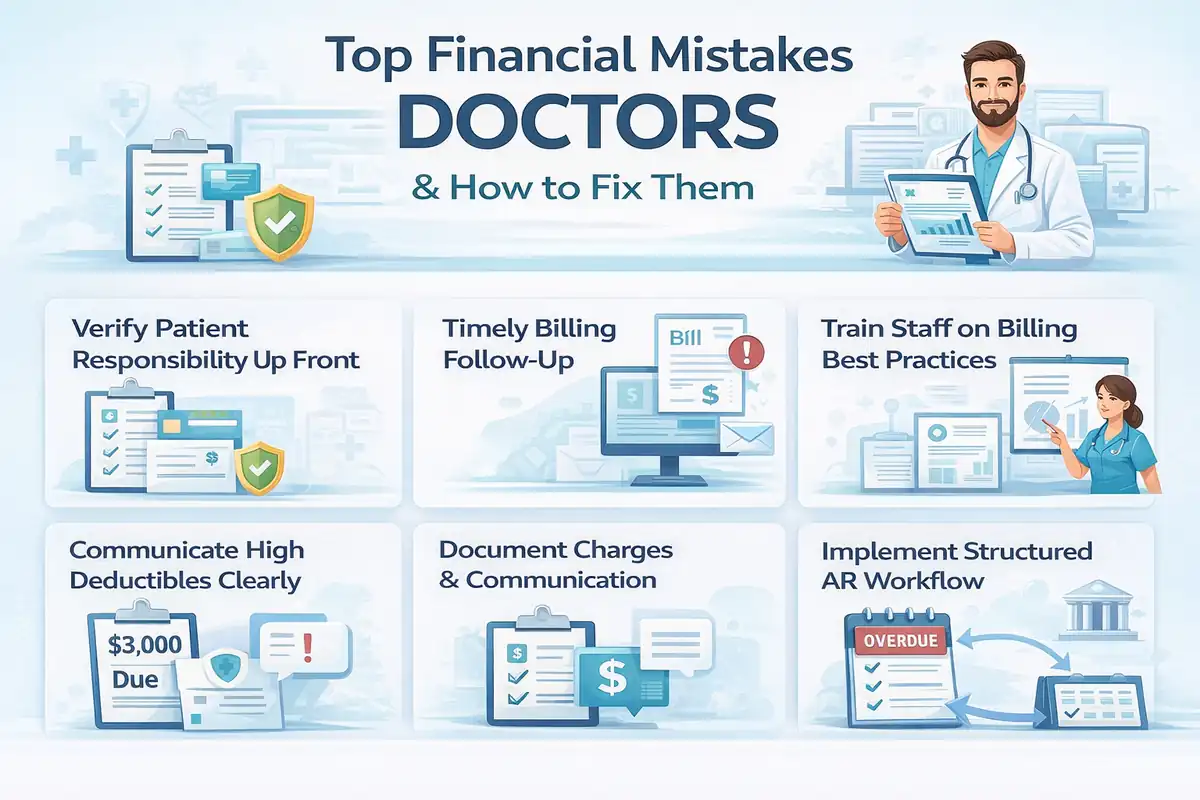
For the majority of clinics the bulk of expenses will cover wages and benefits. How can clinics make sure that they are spending wisely here? A clinic’s primary focus should be on efficiency and productivity – ensuring that members of staff are performing to the best of their capabilities so that they can provide the best quality service in the shortest period of time.
Potential time and energy ‘drains’ – distractions, inefficient tools and equipment, poor communication, to name a few – have been known to interfere with staff productivity. To reduce the amount of time spent on unnecessary tasks, a clinic’s work team must be able to take responsibility for the quality of their work as well as learn when to delegate or ask for help.
One of the key area which is often overlooked by managers and owners-operators is instilling into their employees a sense of ownership in the business and its operations. A professional front-desk receptionist, as well as diligent medical assistants, focus on optimizing their own work by taking advantage of the tools at their disposal, their own time-saving micro-planning skills as well as shortcuts provided in the daily workflow.
One of the most valuable assets in a company is an employee who is aware of the costs of their labor to the company and tries to give back as much as they receive. Make sure your managers learn to value the loners or rule-breakers who don’t seem to follow minor policies and procedures but add to the bottom line time and again. They’re some of the biggest contributors to your cost-saving attempts.
Some employees deliver their best work in structured, disciplined environments, while others are just as efficient by organizing themselves to create a more personal, albeit highly efficient environment, which from the outside may seem odd, even rebellious, but that, in the end, is conducive to successful completion of their tasks. Always provide a medium for honest feedback from your employees since they’re often the most qualified to clarify where time and resources are being wasted.
Investing in training could be the key to unlocking your employees’ potential, and studies show that increased responsibility boosts workers’ morale and sense of job satisfaction.
Equipment
As well as training, clinics must be willing to invest in quality equipment. Providing members of staff with the best tools and equipment will allow them to perform their duties efficiently and on-time. As the saying goes, you must spend money to make money. If you do need to spend it, make sure you either invest in long-term solutions which new and veteran employees can use with ease or in good software for one essential aspect of your business, such as accounting or compliance.
When buying clinical equipment, if there’s no extra money in the budget for shiny new machines, make sure that the second-hand options you look at have some warranty. Some second-hand products may be as good as new, while others may be at the end of their lifetime. Make sure you are trained and knowledgeable about the specs you need or that at least one of your employees or partners can provide some guidance.
Marketing
Let’s analyze where money can be saved in the black hole of 21st century business: marketing. The majority of commercial businesses need to allocate large portions of their budget to marketing, but clinics can get by successfully without such spending. A healthcare clinic can tap into a key resource: its referral and client network. Medical colleagues in the same field can refer your business to their clients.
You can also offer incentives to your existing clients to refer you to their friends and family – but remember that for this tactic to work, customer satisfaction through quality service is key. Incentives can take the form of rewards; for example, you can establish a ‘member’s club’ or a points system.
The amount of spending on rent and utilities will vary depending on a clinic’s size and location, but as current real estate trends mean that rental costs get higher and higher each year in urban areas, more businesses are moving toward co-working and shared workspaces. Perhaps, it could even make sense for you to share your space (and therefore, rental costs!) with other healthcare practitioners.
Optimizing platforms, applications, processes and services
An important strategic move for any business looking to manage costs is knowing what services to outsource. If time-consuming tasks could be taken care of externally, then your clinic would have more time and space to focus on providing top-quality care and ensuring customer satisfaction. Could your administrative tasks such as bookkeeping or information technology tasks such as data interpretation, modeling and storage, be outsourced? A cost-benefit analysis is instrumental in determining if it’s better to perform these tasks in-house than to contract someone to do it for you.
Another important area of focus should be ensuring the efficiency of processes: from client registration to scheduling, to appointments and follow up or after-care. What processes are in place and are they efficient? How do you define efficiency?
A clinic’s workflow should aim to be seamless, and healthcare technology can play a vital role here. Do you have a system for online bookings? Can patients schedule their own screenings and appointments through a website or a smartphone application? IT tools and software are constantly improving productivity, and enhancing the quality of care provided. AI (Artificial Intelligence) is making it easier to streamline patient flows, leading to scheduling systems that are more simplified yet efficient than ever before. New software and cloud platform technology have also revolutionized healthcare administration, with everything from billing to medical record filing now being taken care of digitally.
The healthcare sector is receiving more attention in recent times as demand is constantly growing for improved access to quality healthcare. Clinics and healthcare services need to evaluate their spending and make sure they are running as efficiently as they can in order to hold their place in a market that is growing more and more competitive every day. Chances are, there’s at least one area where a business can rethink its budget and expenses but there are also risks whenever cutting expenses starts to affect the quality of patient care and patient acquisition. Being frugal with everything may turn out to be very expensive for your company in the long run.