Ambulance & EMS Debt Recovery: Recovering Revenue Without Compromising Community Trust.
For EMS directors and municipal leaders, every siren represents a life-saving mission, but the financial “after-care” is increasingly a crisis of its own. In 2026, the gap between what it costs to roll a truck and what insurance actually pays has reached a critical breaking point.
Critical Warning: Emergency and ambulance services must act quickly to collect unpaid medical bills from patients as their financial condition can deteriorate very quickly following a medical crisis. When a household is hit with sudden, high-cost medical bills, the first 60 days are the “Golden Window” for recovery before competing debts and financial instability make collection very complicated.
Nexa provides 100% reputation-safe, equipped with all 50-state collections license, offering free credit reporting, free litigation, free bankruptcy scrubs, and zero onboarding fees. Secure – SOC 2 Type II & HIPAA compliant. Over 2,000 online reviews rate us 4.85 out of 5.
Need a Collection Agency? Restore Your EMS Cash Flow Today
The EMS Financial Reality (Industry Stats)
The “Ambulance Profit Gap” has widened significantly this year. According to the latest 2026 CMS Ground Ambulance Data (GADCS) and industry benchmarks:
-
$1,526 Under-Reimbursement: On average, across all payers, ambulance agencies are under-reimbursed by over $1,500 per transport compared to the actual cost of readiness.
-
$2,672 vs. $1,147: While the mean cost of a governmental ambulance transport has surged to $2,672, the mean reimbursement across all payers remains stuck near $1,147.
-
37% Emergency Fragility: Recent Federal Reserve data shows that nearly 37% of adults cannot afford a $400 emergency expense. Since the average ambulance bill exceeds $1,200, patients move into financial distress almost immediately.
-
45% Recovery Drop-off: If a patient balance isn’t addressed within the first 120 days, the likelihood of recovery drops by nearly half as patients deprioritize “one-time” emergency costs behind recurring monthly bills like rent and utilities.
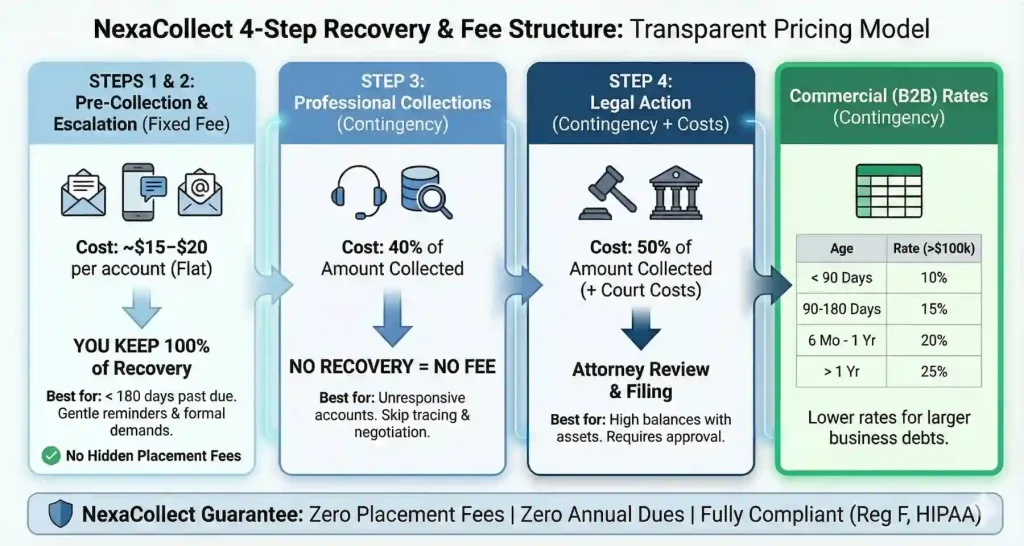
The Nexa 4-Step “Rescue” Ladder
We separate “slow payers” from “bad debt” to maximize your recovery while protecting your department’s community image.
Step 1: The Account Reconciliation (Fixed Fee – $15)
Ideal for accounts 60–90 days past due. Because patients’ financial conditions deteriorate so quickly, this “soft touch” reminder acts as a firm nudge to pay while they still have the liquidity.
-
The Result: The patient pays you directly. You keep 100% of the money.
Steps 2–4: Specialized Medical Mediation (Contingency)
For aged debt or patients who have “ghosted” your internal team. Our mediators use advanced skip-tracing and empathy-based negotiation to find solutions before the patient faces bankruptcy.
-
The Result: You only pay us if we recover your funds. No Recovery = No Fee.
Navigating the Regulatory Landscape
Ambulance collections are a legal minefield. Nexa is hard-coded for 2026 compliance with the newest state laws:
-
Oregon (HB 3243): Effective January 1, 2026, ground ambulances are prohibited from balance billing enrollees for more than the in-network cost-sharing amount.
-
Utah (HB 301): New 2025/2026 laws codify base rates and strictly prohibit ground ambulance providers from charging rates that exceed established caps.
-
Illinois (SB 2405): As of July 2025, non-participating ground ambulance providers must ensure enrollees incur no greater out-of-pocket costs than if the service were in-network.
-
New Hampshire (SB 245): Effective January 1, 2026, this law officially bans “balance billing” for ambulance rides. It also sets mandatory rates for how much companies can charge insurers, significantly changing the negotiation landscape for EMS providers.
-
California (AB 716) – The 12-Month Rule: While active since 2024, California’s law has a strict provision that creditors must know: You are prohibited from reporting adverse information to a credit agency or starting civil action against a patient for a minimum of 12 months after the initial billing. Nexa’s systems are pre-set to respect this “cool-down” period.
-
Maine (LD 1290): Maine now prohibits balance billing for all covered emergency and non-emergency ground ambulance transports. If no local rate is set, the law caps reimbursement at the lesser of 325% of Medicare or the billed charge, requiring precise coding to ensure you don’t over-bill and trigger a violation.
-
Texas (SB 2476): Since early 2024, Texas has banned balance billing for ground ambulance trips. However, in 2026, the focus has shifted to the Independent Dispute Resolution (IDR) portal. If a health plan underpays, we help you navigate the state-mandated mediation and arbitration process to secure the “just and reasonable” rate.
-
Washington State: The Balance Billing Protection Act has been expanded to include ground ambulances. It requires providers to bill health plans directly and strictly prohibits asking patients to “waive” their protections—a common mistake that can lead to heavy state fines.
Recent EMS Recovery Results
-
Private Ambulance Provider (FL): Recovered $280,000 in aged patient balances (120+ days) in just one quarter.
-
Municipal EMS Department (TX): Used our Step 1 Fixed-Fee service to recover $42,000 in “small balance” co-pays that had been sitting idle for six months.
-
NEMT Provider (CA): Reduced overall DSO (Days Sales Outstanding) by 32% within the first 6 months.
Frequently Asked Questions (FAQ)
1. Why the urgency?
Patients often experience a “vicious cycle” of financial deterioration after an emergency. If you don’t collect within the first few months, you are often competing with hospital bills, lost wages, and other post-crisis expenses.
2. How do you handle patients with “Insurance Denials”?
We identify if the issue is a simple “claim denial.” Often, we can point the patient back to their carrier to resolve the underlying issue, resulting in your bill being paid by the insurer rather than the patient.
3. What about “Indigent” patients?
We perform “ability-to-pay” scrubs. If a patient is truly insolvent, we provide you with that data so you can accurately classify the debt as “Charity Care” rather than wasting resources.
Need a Collection Agency for unpaid EMS Service bills?Serving Nationwide: Contact us |